Care tactics
In Matthew 25:34-40 Jesus tells us how to put our love for our neighbor in action. The second in a series on the Corporal Works of Mercy, U.S. Catholic takes a look at how modern Christians visit the sick.
ACHOO!
"God bless you."
One of the legends behind saying "God bless you" originates in the belief that a person's heart stops for a fraction of a second during a sneeze. Even though that old wives' tale won't help cure the cold or allergy that caused the sneeze, people continue to say it.
Catholics might offer a different reason for saying "God bless you." The phrase does two fundamental things that Catholic leaders call for when they talk about caring for the sick.
First, it's an acknowledgment. It says, "I heard you." The late Cardinal Joseph Bernardin said one of his basic convictions about the ministry of health care is the idea of "being there." "Illness is a kind of human exile," he wrote in A Sign of Hope: A Pastoral Letter on Healthcare. "We must recognize the absolute necessity of being present as a community to others in need."
Second, "God bless you" means you are blessed. Christians are taught to have the utmost respect for the sick, suffering, and dying. Not only do the gospels speak clearly about Christ's love for the sick, but those who are ill are a reminder of the suffering he endured on the cross.
"You who are weighed down by suffering are in the front line of those beloved by God," Pope John Paul II wrote in an address to the sick and suffering last year. In speaking against euthanasia, the Roman Catholic bishops of Maryland wrote, "By suffering, dying, and rising, the Lord gave the mystery of human suffering and death a profound and salvific meaning."
 |
|
Parish nurse Delma Huggins examines a young patient at Santa Cruz Catholic Church in Tucson, Arizona. |
In witnessing, or being there, for those who are so specially blessed, Catholics can learn more about the words they read in the Bible.
Catholic hospitals and parish groups are challenged to take the extra time that insurance groups don't allow to build relationships with the sick and suffering.
Though hospital stays have been made shorter, pioneering hospitals have found ways to treat not only patients but communities. They've also learned how to build the communities' trust.
Parishes and families have adapted, too. According to the Wall Street Journal, households with at least one adult providing elder care have risen from 7 million in 1987 to 22.4 million today.
Mary Kilcline will never forget Brother Dan who came to visit her sick mother. "He had this great Irish face," says Kilcline. "He put his two hands around my mother's face and said, 'God's just going to put his arms around you and take you right up to heaven.' I reminded her of that all the time."
Kilcline who had been a nurse at a doctor's office for 12 years, quit her job when her mother, Mary Siemion, became ill. Siemion lived with Kilcline for two years before she died last March at age 84.
In the last five years of her life, Siemion's husband, son, and sister died. She was in and out of the hospital four times. She moved in with her daughter, had a stroke, and fell down and broke her nose. She couldn't remember things and she couldn't walk. She was too sick to go to her sister's funeral. Everything in Siemion's life had changed rapidly, and for the last six months, she knew she was going to die.
Bernardin said ministers of care help bring order to the chaos of illness. "God looked at creation and saw that it was good," Bernardin wrote. "We are reminded that God gives order, meaning, and purpose to the chaos that at times surrounds or invades our lives."
|
|
|
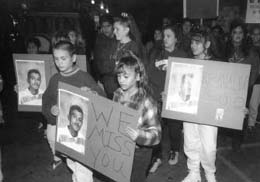
Wanting to heal the community, as well as the sick, the staff of St. Mary'sCarondelet Health Network held a peace walk against violence. |
Parishioners who give hospital and home visits to the sick in Kilcline's parish, St. Daniel Catholic Community in Clarkston, Michigan, are trained to make their visits at the same time every week. Being reliable and predictable helps ministers of care build a respectful relationship with the sick person.
Kilcline, who had been a churchgoer at St. Daniel but never a volunteer, quickly saw the peace brought to her home during visits from Brother Dan and parishioners and decided to become more involved in her parish as a eucharistic minister. As her mother's illness worsened, Kilcline assumed the job of bringing her Communion.
Sometimes her mother would cry. "I'd say, `You didn't tell me it was our crying day. I want to cry, too. And she would laugh, and I would hold her hand," says Kilcline.
Brother Dan visited Kilcline's mother again just hours before she died. "It was amazing," says Kilcline. "All day long she had been struggling to catch her breath. He said, 'You have to tell her it's okay for her to go; she's waiting for you to say that.' It was hard, but I told her. After he left, she was just very peaceful. No struggling."
By spending time with her ailing mother—styling her hair, shopping, talking about what kind of music to have at the funeral—Kilcline learned the art of listening. Patience and listening skills are the key elements to being a good visitor to the sick.
Kilcline can already see that her visits are doing good for others who are sick. "I'm amazed at how good I am. It must be my mom working for me up there," she says.
Kilcline isn't planning to return to work because visiting the sick is "something I have to do for myself."
"You just get such reward from it, it's so fulfilling," she says. "I feel my faith is absolutely stronger."
A matter of community
In trying to improve a parish nurse program that better serves poor, Hispanic neighborhoods in south Tucson, Arizona, St. Mary's Carondelet Health Network, a Catholic hospital, trained professionals to fight and prevent disease. But the professionals also took on new roles: fighting and preventing crime.
"The children say their major health concern is being shot," says Kathy Michaels, Carondelet's director of community outreach.
Working from the idea that you cannot cure an individual without curing the community, the staff of the parish nurse program, which started out as a makeshift clinic in 1991, held a peace walk against violence. On a Friday night last December, 558 neighbors walked down South Sixth Street, labeled by Tucson police as the city's deadliest.
Parish nurse specialist Isela Luna said the peace walk has a lot to do with the success of the parish nurse program. Nurses listened and responded to the community's needs. And being there for the community earned the Carondelet Health Network program neighborhood support.
"[The peace walk] could have easily turned into a political rally," says Luna. "But we wanted to focus on spirituality."
According to Luna, who was born and raised in Mexico, a feeling of trust is especially important in the Mexican American culture. "Building a community is something you must do. It's not an option."
Changes in welfare reform and immigration laws will greatly affect the Hispanic population Carondelet is trying to serve. People who earn more than $3,588 a year, well below the poverty level, are no longer eligible for Medicare in Arizona. And until now, legal U.S. residents were never required to be citizens in order to receive health benefits, says Luna. "We are planning a health fair in October to encourage people to become U.S. citizens on the basis of how it will affect their health."
Cultural beliefs are also a health risk. "There is a belief in whatever God wills," says Michaels. As a result, Mexican Americans are often sicker and more difficult to manage by the time they seek care, she says.
Only through strong relationships can nurses help patients with issues such as deciding they need to go into a nursing home because they can't maintain their home. "You can't tell someone that. They need to see it for themselves," Michaels says.
Like the practice of saying "God bless you," building relationships might have little to do with finding a cure for cancer or the common cold, yet people continue to do it.
Three parishes within seven blocks of one another provide space for the parish nurses to serve poor residents. A bilingual staff at the parish clinics perform services, including ear exams, blood-pressure checks, vaccines, screenings for breast and cervical cancer, and testing blood-sugar levels for diabetics. At one of the chapels, those waiting for service sit in the pews.
"Parish nursing has had a kind of resurgence, yet in terms of our history, it's a very old idea," says Michaels. "The way I see it, you can't take a community outreach program and put it in a parish and call it a parish program."
All the nurses in the Carondelet Health Network must be members of the parish communities they serve. And besides promoting healthy lifestyles, making diagnoses, and stopping the progression of disease, parish nurses from Carondelet spend time praying with people and reading religious passages.
"A strong component of health is spiritual strength, no matter what faith. It has a physiological component. Pills and surgical intervention aren't going to work as well if you don't feel safe and trusting," says Michaels. "Some people are into giving advice and telling you what you need, rather than being in a two-way process. Providers who are skilled at establishing relationships are worth their weight in gold."
By Mariana Farrell, a copy and design editor for the Post Tribune in Gary, Indiana. This article appeared in the September 1997 issue of U.S. Catholic.
Making house calls
"The prayer of faith somehow sustains me," said Sister Thea Bowman, F.S.P.A. while battling cancer. Bowman, a gospel singer, evangelist, author, teacher, and recipient of the 1989 U.S. Catholic Award for furthering the cause of women in the church, spent her life preaching the Word of God. And when she discovered her illness, the preaching didn't stop. Bowman offered words of hope, courage, and love to the sick and dying: "To the suffering I say: 'Try to reach out to others. Try to let people know how much you love them. Try to maintain a sense of humor and laughter in your life.'" To the healthy, Bowman said, "listen to the sick, learn to read them, and be gentle."
Bowman died on March 30, 1990 two weeks after U.S. Catholic interviewed her. The following is an excerpt from that interview, which originally appeared in June 1990.
How can healthy people treat the sick better?
It's important for the healthy to listen to the sick. They should ask: "How can I help? What can I do? Would you like me to sit with you a while? What do you need? What do you want? Are you tired? Do you need to rest?" These seem like really simple questions, but they are seldom asked.
If and when the questions are asked, it's also important for the asker to listen to the answer. Somebody came to visit me a while ago and asked, "What do you need?" I said some grapefruit. So the person went out and bought grapefruit and plums and apples and bananas. It was nice, but all I wanted was grapefruit. That's what I mean about listening to what the sick person asks of you.
Learn to read the sick. If you're perceptive, you can tell when someone is tired and needs rest. Forget your own agenda when you go to visit a sick person. If the sick person is having difficulty talking, unless you're sure he or she has something to say and wants to talk, don't make the person talk and don't put the sick person in situations where he or she has to talk.
The healthy must understand that the sick are very sensitive—sensitive to noise, sensitive to touch. People will come and pat me, but because I have bone cancer, I'm very sensitive to touch. So people won't even realize they're hurting me. Read the sick person's face and body language. Try to understand where the sick person is coming from. Be sensitive to the need for a quiet and peaceful environment. Don't overload sick people with distractions and noisy actions. Be gentle.
Be sensitive to the sick person's caretaker, too. Ask the caretaker if he or she needs help cooking meals or some time to rest. Another thing: don't offer to help if you don't want to help. Don't make promises you can't keep because the sick person and caretaker will wait for you.
What if someone says, "I want to help, but I just don't know how to help"?
Then it's up to the sick person to say what he or shereally needs. My advice to sick people is: tell people what you really want. I used to be reluctant to do that, but if someone wants to do something for you, that person is going to do it regardless; so the best thing to do is to tell them straightforwardly what would be the most helpful thing to do. I might say, pray with me or sit with me. Or I might need someone to read to me or rub my foot.
The basic thing that I'm saying to both the sick and the healthy is: keep the lines of communication open. Otherwise some things that need to be done remain undone or things that are done are not helpful or are actually hurtful.
So the sick and the well do have something to offer each other?
Yes. The two can offer each other love, comfort, laughter, perspective. Illness can distort perspective, and the person who is sick needs the perspective of the well community. I need the perspective of little children and the elderly and of people who are facing life every day. But illness also helps clarify perspective. People who are well can learn from the sick new ways of thinking, relating, and accepting.
Sick people can teach the well an appreciation for health and movement and life. The sick can share insight into what it means to live, what it means to suffer, what it means to face death. The lines from a traditional song of the black community come to mind: "I'm going to sit at the welcome table. I'm going to drink from the golden fountain. I'm going to my sainted mother. I'm going to meet with my friend Jesus one of these days."